I Work At A Women’s Clinic In Post-Roe America. This Is What I Wish Every Teenager Knew.
I was in the clinic the day Roe v. Wade was overturned. I was either inserting an IUD, treating another case of chlamydia or ordering breast imaging after finding a nut-like lump during a routine breast exam. Perhaps I had just finished counseling a woman about what to expect after taking her medical abortion pills.
Even though the entire staff at my nonprofit feminist health center in Chico, California, knew this was coming, the news still hit like a blow. I had spent 26 years of my life dedicated to empowering women about their health and reproduction, and in one terrible decision, the Supreme Court sent the rights of women in America about 70 years backward.
Advertisement
I became a contraception expert almost by accident. I am a certified nurse-midwife, and in 2017, after years of providing home birth midwifery care, I decided to try a clinic job. Delivering babies as a solo home-birth midwife is one of the most meaningful things a person can do for a living. Midwives are honored to be present at life’s greatest and most intimate transformations. But the work also involves getting called out of bed in the middle of the night, strings of lost nights of sleep and high-stakes stress when unexpected complications arise. Not to mention always being on-call. I was ready for a change. One of the benefits of a career in nursing is that you can work in many different capacities and settings yet stay within your profession.
When I took the position at Women’s Health Specialists, I found that my own reasons for going into women’s health were perfectly aligned with the clinic’s mission: “Working toward a world where women control their own bodies, reproduction and sexuality.” The clinic is dedicated to providing women-controlled health care and advocating for all options for all women, with the understanding that only with dignity and freedom of choice can women achieve their full potential. I felt like I was home.
Advertisement
Compared to attending births, my role as clinician here initially seemed easy, with daytime hours and a set schedule. The patient visits I conducted were “basic” for someone with my level of training and experience. They included help with contraception and sexually transmitted infections, general gynecological care for mostly teens and college students, counseling on pregnancy options, and medical abortion.
I would soon discover that my patients needed so much more than basic clinical care. For one thing, anyone who came through our doors would be seen, regardless of ability to pay. We saw young, old, people who were unhoused and years behind on regular health care maintenance, and undocumented immigrants afraid to go anywhere else. Our waiting rooms were lively and colorful, with all genders and sexual orientations and different crowds that comprised our college town and the surrounding farming communities. Everyone knew that for sexual health needs, our clinic was the place to go.
Advertisement
Clinic days were hectic because I would often see 35 or more patients in a day. When I walked into an exam room, I had 15 minutes face-to-face with a person, and that often included a physical exam. I saw my work as a privilege and a responsibility, and I wanted to make each visit a meaningful interaction for the patient. This meant really listening to them and giving counsel that was accurate and nonjudgmental. I wanted my patients to leave the clinic feeling better about themselves than when they came in.
Then there was the fact of the world dramatically changing outside our clinic walls.
Donald Trump was inaugurated as president three weeks after I started my job, and with his ascent came immediate threats to women’s rights and autonomy. That is when we saw a massive uptick in teenagers getting IUDs. They wanted to have contraception that would last his whole presidency, just in case. I will never forget the first 14-year-old I helped to get an IUD. She was so brave and happy about it, having made that choice for herself.
Two years of pussy hats and women’s marches later, on Nov. 8, 2018, our neighboring town of Paradise burned down in a single, historically destructive day. Thirty thousand people lost their homes in the Camp fire. We stayed open extra hours for days afterward, our clinic blanketed in apocalyptic black smoke, daylight reduced to a dim red haze, so that hundreds of people could replace birth control that had been lost in the fire. Even still, there was a huge surge of unintended pregnancies in the fire’s aftermath.
And then came the pandemic. We never closed our doors, not even for a single day ― because guess what people locked down at home do more of? Everyone and their aunties got urinary tract infections or needed birth control. Our community saw a rise in syphilis cases during the COVID years, which we called the Second Epidemic. Our services were essential, and to continue providing them, we risked bringing the deadly new infection home to our families. I was proud to be a pilot provider of telehealth medical abortion. The data from our clinic’s pilot program during COVID helped determine that telehealth abortion is safe so that this service can now be scaled up to serve people in states with bans on physical abortions.
People seeking our care were often in trouble and needing serious help. Perhaps they were a victim of sexual assault or had been betrayed by a partner and left with both a pregnancy and an STI. People came in with multiple concurrent STIs, or a breast mass or a lump in their ovary the size of a cabbage. A woman came in bleeding from what turned out to be a ruptured ectopic pregnancy. I had never seen one before, but I swiftly diagnosed it, saving her life.
Advertisement
There would also be hundreds of routine visits ― injection after injection of Depo-Provera birth control, contraceptive pill prescription after prescription, and complaint after complaint of “funky discharge,” the hallmark of vaginitis. I counseled patients about the same topics day in and day out ― safe sex, how to use each birth control method correctly and the care of one’s vagina. I became skillful at addressing delicate personal and sexual issues that are cloaked by our culture in stigma and shame. I shared as much information as I could stuff into each encounter so that women would leave a little more empowered to take care of themselves. I often thought that I should put all of this in a book.
Kirsten Clodfelter
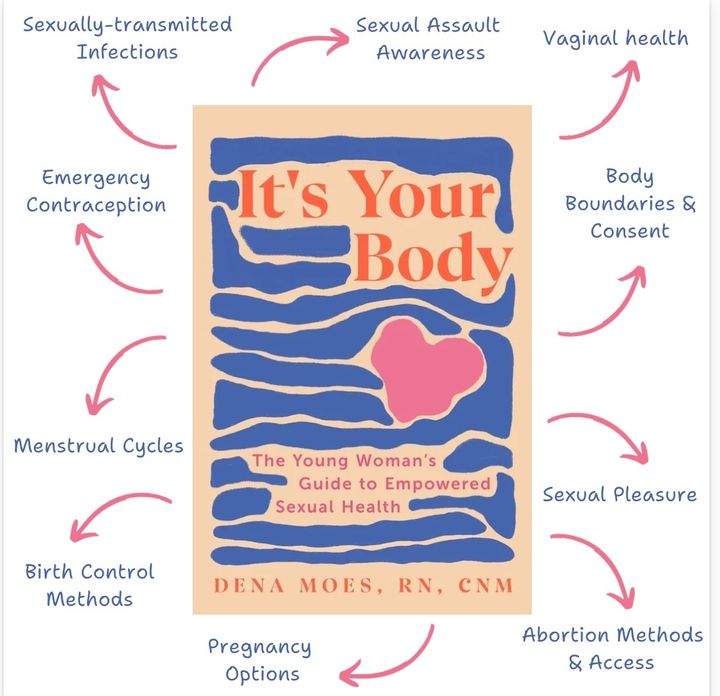
As an expert in all things contraception and reproduction, I also felt I had a responsibility to help young people during the transition to a post-Roe America. Teenagers are especially vulnerable to the consequences of unintended pregnancy. Around the country, they now face abortion bans and care deserts, fake clinics and misinformation circulating on the web. These are all barriers to reproductive autonomy. I decided to write “It’s Your Body: The Young Woman’s Guide to Empowered Sexual Health” because everyone has the right to decide whether, when and with whom they have a baby.
As fall approaches, the Center for Reproductive Rights reports that 6 million college students are heading to campuses in abortion-restricted states. Fifty-five percent of them are female. Abortion care is now fully illegal in 14 states, many of which have historic and large universities, including Florida, Texas, Georgia and Indiana. Young people are the hardest hit by abortion bans as they are the least likely to have the resources required to travel out of state for help. The consequences of being denied abortion care as a student have been found to lead to an incomplete education, falling into and remaining in poverty, and the increased likelihood of experiencing domestic violence. This is a public health crisis for the young women of America.
I cannot change the laws or replace Supreme Court justices or reopen closed clinics in states far from my California home. But I could pour what I know from years of clinical practice into a resource guide for teens and young adults. I could provide information on how to obtain medical abortion pills online or by mail, and how to take them correctly and safely. My hope is that the information in my book will help teenagers and young women make their own decisions about their bodies, their fertility and their lives.
Advertisement
Do you have a compelling personal story you’d like to see published on HuffPost? Find out what we’re looking for here and send us a pitch at pitch@huffpost.com.

Comments are closed.